As a Registered Midwife I am an autonomous primary healthcare provider to pregnant women, postpartum women, and their newborns (Practicing Midwifery In BC, 2015). In this care model, a woman’s maternity care is provided by her midwives with: appropriate interprofessional engagement of lab and ultrasound services, admitting and discharges to hospital, and consultation with peers such as nurses, obstetricians, and pediatricians. For healthy low risk women, we conduct their antenatal visits, delivery, and postpartum care. This is tightly regulated by the CMBC in order to keep safe parameters; this includes regulation of equipment, medications, emergency skills, and transportation plans for planned home birth (Standards and Policies, 2015).
The model of midwifery care allows for a close intimate patient-care provider relationship throughout the childbearing year. The nature of this care has many benefits, but one the greatest benefits, I argue, is for women experiencing Major Depressive Disorder (MDD) in pregnancy. Perinatal services estimates that up to 1 in 5 women will experience an episode of depression in their pregnancy (Williams, 2014). While this rate is similar to the non-pregnant population, the clinical significance and concerns with MDD during pregnancy is heightened.
I believe that the continuity of care provided by midwifery allows for early detection, frequent care provider access, and a trusted care provider. Nonetheless, there are potential concerns with the midwifery model in regards to: curation of resources used to inform practice, professionalism, and engagement with patients online. As we will explore in this blog post, MDD is a chronic disease that can be well illustrated using both determinants of health and a multi-level of influence lens, that also happens to impact vulnerable populations.
Professionalism and Social Media
Midwives, like all professionals, find themselves facing duality in caring for their patients. When not at work, they are members of the public. They must find the balance between the recommendations of their college and their personal desire to be present members of the community. Personally, I have chosen to approach this by keeping some separation between professional and personal identities online; a challenging task for midwives who work closely with families throughout their childbearing year. When care reaches it’s inevitable close at six weeks postpartum, many patients, and admittedly midwives, are not ready to end their relationship in totality. Connecting online can allow for the fostering of genuine relationships outside of care, but can also easily deviate into inappropriate care interactions. For mothers facing depression in their pregnancy and beyond, having clear boundaries from their midwife, along with appropriate referrals, is necessary to avoid potentially harmful interactions. The CMBC has provided guidance on this by stating that midwives should not accept, nor extend, invitations of clients currently in care (“Policy on Appropriate Client-Midwife Relationships”, 2018).
Curation of Resources for Practice
Evaluating the quality of evidence available online requires evaluating each search result; a time consuming and cumbersome task amidst a bustling clinic day. For this reason, I use UptoDate for many clinical information quests. UptoDate is a database for healthcare providers to utilize synthesized evidence-based summaries of medical topics, available at the point of care (Product, 2018). However, in embarking on curating resources, the need to have a “hub” for resources not located on UptoDate became apparent. After considering several platforms, I selected Pinterest for it’s clean interface, and ability to subdivide into categories (Healthcare, Policy, and Education, 2018). This allows me to neatly gather my curated resources for care topics such as MDD all in one place.
Defining Health
Before we dive deeper, I think it’s important that we take a step back and critically look at how we define “health”. The World Health Organization’s (WHO) Constitution defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (Constitution of WHO). Established shortly after the end of World War II in 1948, this definition has not changed for seventy years. While acknowledging the multifaceted nature of health, its use of the term “complete” make it challenging to see this definition as helpful or relevant to today. Criticisms of the WHO’s definition include that it medicalizes society, does not reflect advances in healthcare for those aging with chronic disease, and poses problems for application and measurement (Huber).
When one uses the term “complete” it implies that anything less than a perfection in any one of these areas is a perpetual state of unhealthy (Jadad). In turn, this supports the advancements of pre-illness technologies. While this might increase the rate successful treatment of illness in a few individuals, it subjects large numbers of the population to treatment where the risks may outweigh the benefits (Huber). This is a concept that percolates into all areas of healthcare, including mental health. One example of this may be the lower threshold for use of antidepressant medications in newly diagnosed cases of MDD in pregnancy; in an earnest attempt to make women feel “complete”. The use of medication may occur before the use of lower risk therapies such as Cognitive Behavioural Therapy (CBT), or bright light therapy (Williams).
Determinants of Health, Chronic Disease, and Multiple Levels Influence
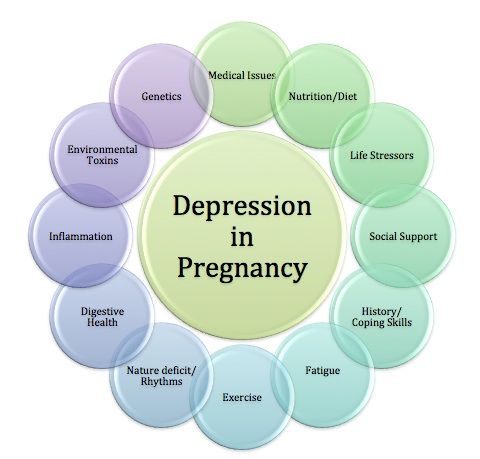
There are several chronic diseases that are relevant to my practice, but mental health is the most commonly encountered. MDD is the most observed. Mental Health is a Chronic Disease of focus at the national and provincial level (Public Health Agency of Canada, Williams). Determinants of health that impact MDD include: Income and Social status, Social Supports and Coping Skills, Biology and Genetic Endowment, and Culture (Williams). Many of these determinants can factor into a pregnant person’s level of stress, and ability to cope on an ongoing basis with life’s stresses.
For women taking medication for MDD, some will change medications: prior to becoming pregnant, in early pregnancy, or wean from their medication. Although there are safe medication options in pregnancy, many women feel stigma around taking antidepressants in pregnancy. Supporting women to continue their medication, adjust dosages appropriately, and engage in CBT exercises (Haring) is a role Midwives fill for managing MDD as a chronic disease.
As I’ve alluded to, there are also multiple levels of influence on MDD. Most prominently are “individual lifestyle factors”. Behaviours such as exercise, sleep, and nutrition are often recommended for MDD treatment. While pre-pregnant (or postpartum) women may succeed in these strategies, pregnancy challenges a woman’s ability to: exercise, sleep, and eat as she usually would. All of these lifestyle changes could theoretically place women at higher risk of experiencing depression, and reduce the efficacy of CBT. Moreover, the level of “social and community networks” influences MDD for some women, including single mothers. An unintended pregnancy may cause drastic changes in relationships with those closest to her. This change in her social network may also increase her risk of depression (Williams, 2014).
Aboriginal and Vulnerable Populations
British Columbia and Ontario both have dispersed populations, with density around major city centers. Due to this, both provinces have identified specific populations who experience poorer health than other British Columbians (PHSA, 2011). The Provincial Health Services Authority (PHSA) identifies those populations as those: living in poverty, with mental health or substance abuse, aboriginal peoples, immigrants, and refugees (PHSA, 2011). However, unlike Ontario, British Columbia has prioritizes Aboriginal Health; with particularly attention on the well-being of infants, children, and families. This mostly targets rural populations, and those living on reserve. Aboriginal populations overall rank lower on the education, and higher in unemployment compared to non-aboriginal Canadians (NCCAH, 2013).
Provincially and locally we have several resources and guidelines geared towards Aboriginal moms and babies: these include the Friendship Center (provides drop-in programs, including lunch for families), Aboriginal specific “Pregnancy Passport”, “Safe Sleep Toolkit” and Reproductive Mental Health’s “Emotional Health Guide”.
Future Directions
As we look ahead to the future direction of Major Depressive Disorder in pregnancy, I feel there is a need for further research at the level of “general socioeconomic, cultural, and environmental factors”. A systematic review from Scotland concluded that the evidence doesn’t support specific interventions for the prevention of MDD during pregnancy, unless identified risk factors are present (SIGN, 2012). I argue that this is short sighted. As we have seen, assessing risk factors requires looking at determinants of health, multiple levels of influence, and analyzing the interconnectedness between MDD and vulnerable populations. While SIGN factors in a woman’s personal and family medical history, and contributing risk factors from individual, social, living conditions factors, it fails to consider general socioeconomic, cultural, and environmental factors as risk factors for, or associations with, depression in pregnancy. For example, it does not include exploration of concepts such as how colonialism may impact MDD rates among Aboriginal women, or how cultural norms around: gender, “motherhood”, and the identity of “mother” may contribute to MDD. Using this level of influence to further explore depression in pregnancy may allow us to discover evidence that does in fact support specific interventions for prevention in specific populations. In the vacuum of better evidence, I feel the midwifery model of care is an ideal fit for women experiencing depression in pregnancy as it allows for identification of known risks. However, our guidelines are only as good as the literature used to create them, and ultimately, we must strive for better research.
References
College of Midwives of British Columbia. (2018, May 4). Policy on Appropriate Client-Midwife Relationships [Press release]. Retrieved from http://cmbc.bc.ca/wp-content/uploads/2018/05/Policy-on-Appropriate-Client-Midwife-Relationships.pdf
CMBC. (2015). Career as a Midwife. Retrieved from http://cmbc.bc.ca/registration/general-information-faq/career-as-a-midwife/
CMBC. (2015). Standards and Policies. Retrieved from http://cmbc.bc.ca/standards-policies-forms/standards-policies-and-forms/
Huber, M. (2011). Health: How should we define it? British Medical Journal, 343,(7817), 235-237. https://doi.org/10.1136/bmj.d4163 (link http://www.jstor.org/stable/23051314)
Jadad AR, O’Grady L. (2008). How should health be defined. British Medical Journal, 337 (a2900).
Pinterest. (2018). Healthcare, Policy, and Education. Retrieved May 13, 2018, from https://www.pinterest.ca/meghan_price_/healthcare-policy-and-education/
Public Health Agency of Canada. (2015). Report from the Canadian chronic disease surveillance system: Mental illness in Canada, 2015. Retrieved from: http://healthycanadians.gc.ca/publications/diseases-conditions-maladies-affections/mental-illness-2015-maladies-mentales/alt/mental-illness-2015-maladies-mentales-eng.pdf
Romm, A. (2018, January 30). 10 Natural Approaches to Depression in Pregnancy. Retrieved from https://avivaromm.com/depression-in-pregnancy/
Scottish Intercollegiate Guidelines Network (SIGN). (2012, March). Management of perinatal mood disorders. Edinburgh: SIGN; 2012. (SIGN publication no. 127). Retrieved from http://www.sign.ac.uk
